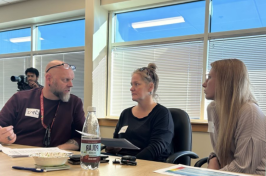
Crisis responders consult with each other during a recent in-person training of the New Hampshire Rapid Response team. The state has partnered with UNH to develop a comprehensive statewide training and certification program to help bolster the state's pool of crisis responders.
New Hampshire's Rapid Response mobile crisis response teams are on the front lines of the state’s mental health and substance use crises, providing immediate support to individuals experiencing a crisis in their communities.
These responders come from diverse training backgrounds and work in pairs, often teaming up with professionals like peer support specialists or clinical responders to assess situations, de-escalate tensions and stabilize individuals — all without relying on hospitalization or law enforcement intervention.
However, these teams have faced two significant challenges: providing high-quality, standardized training across the state and addressing a shortage of crisis response professionals. To tackle these issues, the University of New Hampshire's Institute on Disability (IOD) has partnered with the NH Department of Health and Human Services (DHHS) to develop a comprehensive statewide training and certification program.
In the short term, the program guarantees that all crisis responders receive consistent training no matter where they serve. In the long term, it aims to attract new professionals into the field, build a pathway to careers in behavioral health and help alleviate the statewide shortage of crisis responders.
“Our rapid response teams are sorely understaffed, and for the program to function as designed and intended, we need staff,” says Elizabeth Grosso, director of training and co-lead of the N.H. Rapid Response Crisis Training program at the UNH IOD. “We have a statewide, nationwide mental health access crisis happening right now, and we need to build a bench of crisis responders. We can't rely solely on master's level clinicians because there just aren't enough of them.”
Grosso says the training program has the potential to increase the pool of crisis responders because the curriculum is designed in a way that individuals, including UNH students, with no background in behavioral health can get the knowledge they need to serve as crisis responder.
Those who complete the training earn a UNH digital badge and can apply for crisis responder positions, where they’ll be mentored and complete additional training, resulting in an additional UNH digital badge and certification as a N.H. Crisis Responder.
What the Training Program Entails
Previous training for crisis responders required participants to take a 40-hour, fully online course on their own time. However, the training put together by UNH IOD uses a hybrid model that is more engaging and comprehensive. The 41-hour, 15-week training program uses online coursework, five in-person seminars (10 hours total), and a mentorship component for ongoing support and application of best practices. 
Topics covered in the curriculum include behavioral health crisis intervention, trauma-informed care, community-based support and de-escalation techniques, to name a few.
"It's ideal for a training program like this to be integrated within the university ecosystem because we anticipate that some certified crisis responders will use this pathway to continue their education, whether pursuing a bachelor's degree, or a master's in social work or mental health counseling,” Grosso says. “We also want the pathway to be bidirectional—after having a positive experience with us and getting hired onto a Rapid Response team at a mental health center, responders can advance into different roles while being supported in furthering their education."
Voices from the Field
Most involved in the training agree that in-person seminars are among the program's most significant benefits. For the in-person sessions, the cohort is divided into two classes led by clinical experts and peer advisors who have lived experience in behavioral health challenges and crises.
Lauren Swift and Chris Grasso are peer advisors leading the training.
Swift, who works at Northern Human Services in Wolfeboro, says peer support specialists like herself offer unique insights from their personal experiences with behavioral health and crisis response.
"The clinicians speak from their expertise, and then I add the peer perspective, which brings a different dimension. It’s not about diagnosis; it’s about connection and understanding the crisis itself,” Swift says. “That balance allows us to give trainees a more rounded view of how to engage with people in crisis, blending clinical approaches with lived experience."
Swift typically responds to crisis calls with another peer support specialist, and a clinician is brought in via telehealth if needed.
“We’ve seen a lot of success with this approach. Spending time with individuals, helping them de-escalate and guiding them from fear to hope has been incredibly effective,” Swift says. “We don’t have to send doctors, ambulances or clinicians to every crisis scene. We can send out peers trained for these situations to bring people to a place where they can get additional help and stabilization.”
Grasso, a peer support facilitator for Lakes Region Mental Health Center in Laconia, says one of the strengths of the new training is bringing together the 10 community mental health centers, allowing them to share practices and learn from each other’s experiences.
"It's priceless to see how different community mental health centers handle calls and situations,” Grasso says. “We’re all working within the same program but in different ways. Learning from each other’s successes and challenges helps us adapt and improve how we respond to crises."
Grasso says the mobile response teams have already made a considerable impact and stresses that this training is important because the need for help isn’t going away.
"The need for mental health services is only growing, and mobile crisis teams are making a real difference. By providing safety plans and temporary therapy, we’re helping people avoid hospitalization,” Grasso says.
Swift hopes that crisis response training will someday become as common as cardiopulmonary resuscitation (CPR) training — something people are willing to be proactive about.
“Just as knowing basic CPR can save lives, recognizing the warning signs of suicidality, mental health crises or substance use could help us prevent many tragedies,” Swift says. “Everyone experiences crises at some point. If you can find someone who's never faced an adverse situation that felt overwhelming, I'd love to meet them. We all go through tough times, and we need to remove the stigma around seeking help ... imagine the potential of the people who, if supported through their darkest hours, could go on to achieve great things.”
-
Written By:
Aaron Sanborn | Peter T. Paul College of Business and Economics | aaron.sanborn@dos5.net